
They noted that this area also includes a genetic variant associated with increased levels of interleukin-6, which plays a role in inflammation and may have implications for COVID-19 as well. The researchers did find evidence suggesting a relationship between blood type and COVID-19 risk. Whether you are classified as an A, B, AB, or O blood type, depends on how your genes instruct your blood cells to produce (or not produce) a certain set of proteins. The other association signal popped up on chromosome 9, right over the area of the genome that determines blood type. It also encodes a collection of chemokine receptors, which play a role in the immune response in the airways of our lungs. For instance, this portion of the genome encodes a transporter protein known to interact with angiotensin converting enzyme 2 (ACE2), the surface receptor that allows the novel coronavirus that causes COVID-19, SARS-CoV-2, to bind to and infect human cells. One of them is found on chromosome 3 and covers a cluster of six genes with potentially relevant functions.
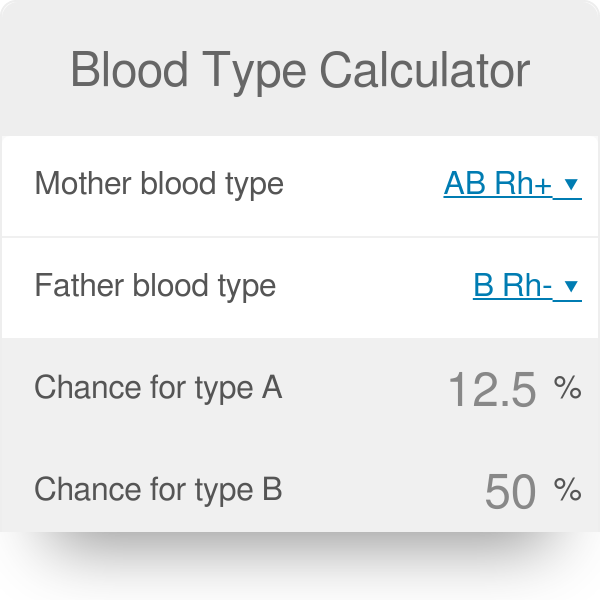
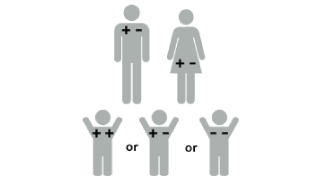
The analysis identified two places that turned up significantly more often in the individuals with severe COVID-19 than in the healthy folks. To find them, the researchers compared SNPs in people with severe COVID-19 to those in more than 1,200 healthy blood donors from the same population groups. The vast majority of these single “letter” nucleotide substitutions found all across the genome are of no health significance, but they can help to pinpoint the locations of gene variants that turn up more often in association with particular traits or conditions-in this case, COVID-19-related respiratory failure. In search of gene variants that might play a role in the severe illness, the team analyzed patient genome data for more than 8.5 million so-called single-nucleotide polymorphisms, or SNPs. Their study included 1,980 people undergoing treatment for severe COVID-19 and respiratory failure at seven medical centers in Italy and Spain. These new findings-the first to identify statistically significant susceptibility genes for the severity of COVID-19-come from a large research effort led by Andre Franke, a scientist at Christian-Albrecht-University, Kiel, Germany, along with Tom Karlsen, Oslo University Hospital Rikshospitalet, Norway. In contrast, people with blood type O appear to have about a 50 percent reduced risk of severe COVID-19. In fact, the findings suggest that people with blood type A face a 50 percent greater risk of needing oxygen support or a ventilator should they become infected with the novel coronavirus.
The two stretches of DNA implicated as harboring risks for severe COVID-19 are known to carry some intriguing genes, including one that determines blood type and others that play various roles in the immune system. While more research is needed to pinpoint the precise underlying genes and mechanisms responsible, a recent genome-wide association (GWAS) study, just published in the New England Journal of Medicine, finds that gene variants in two regions of the human genome are associated with severe COVID-19 and correspondingly carry a greater risk of COVID-19-related death. But why does respiratory failure also sometimes occur in people who are young and seemingly healthy?Ī new study suggests that part of the answer to this question may be found in the genes that each one of us carries. It’s clear that this happens more often in men than in women, as well as in people who are older or who have chronic health conditions. But others develop respiratory failure that requires oxygen support or even a ventilator to help them recover.
Many people who contract COVID-19 have only a mild illness, or sometimes no symptoms at all. Caption: Micrograph of SARS-CoV-2 virus particles isolated from a patient.Ĭredit: National Institute of Allergy and Infectious Diseases, NIH


 0 kommentar(er)
0 kommentar(er)
